The 5 Ms of Geriatric Care: What Every New Dentist Needs to Know
One of the first and perhaps most important lessons to learn is that geriatric patients are the most diverse group you will ever treat. Your patients will span decades ranging from those in their mid-60s to those well into their 90s or beyond. Age alone often reveals little about their health, lifestyle, or abilities. The 85-year-old in your chair isn’t just another “elderly patient”—they might be training for their next marathon or managing multiple chronic conditions. Age is truly just a number, and successful treatment demands looking beyond that number to see the whole person.
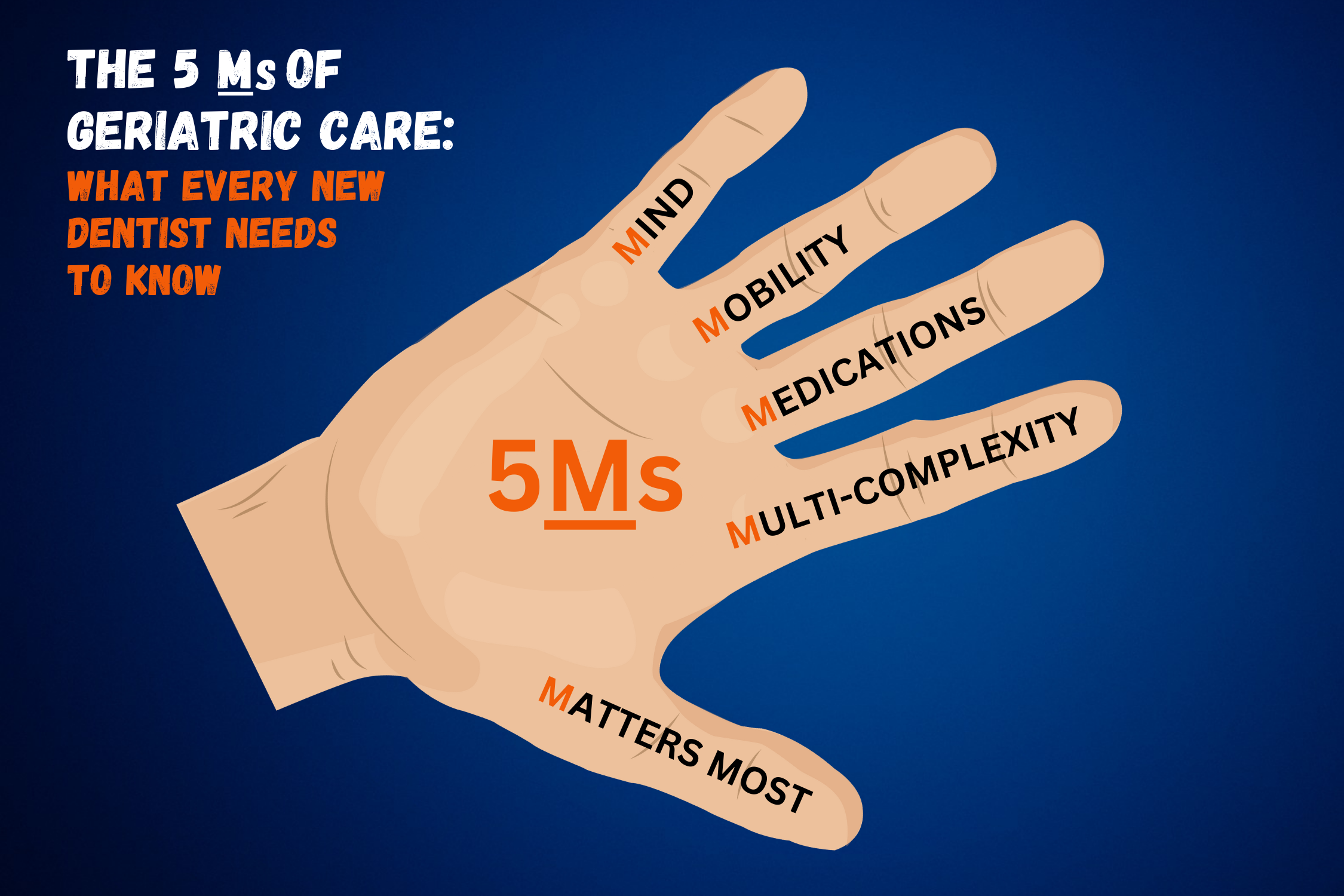
So, how do you navigate this complexity? That’s where the “5 Ms” of geriatric care come in: a framework to help you provide the best possible care.
Why does this matter?
Because successful treatment demands more than clinical skill, it requires empathy and understanding. The 5Ms—Mind, Mobility, Medications, Multi-complexity, and Matters Most—represent the essential aspects of patient care that every dentist should consider when working with older adults. Each “M” is a must, helping you to see beyond surface-level symptoms and build a truly person-centered practice.
Let’s dive into how the 5 Ms can guide you to become a more effective, empathetic, and prepared provider for your older patients.
1. Mind
Cognitive health plays a critical role in a patient’s ability to make informed decisions and follow care instructions. Many older adults experience cognitive changes, from mild impairment to dementia, which can affect their understanding and recall. Engaging caregivers and using techniques like the “teach-back” method—where patients explain instructions back to you—can significantly enhance understanding and compliance.
Tip: Approach each interaction with patience and encourage questions. This builds trust and greatly improves adherence to care. Evaluate a patient’s capacity at each interaction and react appropriately.
2. Mobility
Mobility issues impact nearly every part of a patient’s dental experience, from attending appointments to completing oral hygiene routines at home. Arthritis, muscle weakness, or balance issues may make it challenging for some patients to hold a toothbrush or sit comfortably for extended periods. Short, frequent appointments and introducing adaptive tools like electric toothbrushes and floss holders can empower patients to maintain their independence in oral care.
Tip: For patients with severe mobility limitations, teledentistry can be a convenient option for consultations and follow-ups.
3. Medications
Older adults often manage multiple medications (polypharmacy), which can significantly impact oral health. Common side effects—like dry mouth or increased bleeding risk—necessitate careful adjustments to treatment plans. Be diligent in reviewing each patient’s medications, including over-the counter and herbal products, as these can also affect treatment.
Tip: Collaborate with the patient’s other healthcare providers to ensure safe, coordinated care and minimize potential drug interactions.
4. Multi-complexity
Older adults frequently face multiple chronic conditions, like diabetes, heart disease, or osteoporosis, complicating dental care. For instance, diabetes can increase the risk of gum disease, and certain heart conditions may limit treatment options. Tailoring your care plan to address these conditions and consulting with other healthcare providers as needed—can greatly enhance patient safety and outcomes.
Tip: Set realistic goals that consider the whole health picture, helping patients maintain their oral health while managing other conditions. If you consult with the patient’s other providers, document those discussions in the patient’s chart.
5. Matters Most
This final “M” emphasizes the importance of personalizing care based on what truly matters to each patient. For some, comfort may be the top priority, while others may prioritize aesthetics or specific functional outcomes. Taking time to understand each patient’s values and goals can help you create a treatment plan that respects their preferences and enhances their quality of life.
Tip: Ask open-ended questions to uncover patient goals. This fosters trust and allows for a truly person-centered approach.
Final Thoughts
Geriatric dentistry isn’t about treating old age—it’s about honoring and caring for individuals who happen to be older. Each patient brings a unique health profile, history, and set of values to your chair, and your role is to recognize and respect that uniqueness. By using the 5 Ms framework, you will be prepared to deliver personalized, compassionate care that aligns with each patient’s health, lifestyle, and preferences.